CME/CE Activities
Addressing and Treating Iron Deficiency to Improve Symptoms and Outcomes in Patients with Heart Failure
Format: Webcast
CME/CE Credits: 1.0 hrs
Ironing Out the Data: Iron Deficiency in Heart Failure
Format: Podcast
CME/CE Credits: 0.5 hrs
News Digest
Intravenous Iron Repletion in Heart Failure & the New Generation of IV Iron
Intravenous Iron Repletion in Heart Failure & the New Generation of IV Iron IV IRON: THE STANDARD FOR IV REPLETION IN HEART FAILURE In recent decades, a substantial amount of
Improving Iron Deficiency Detection in Heart Failure
Improving Iron Deficiency Detection in Heart Failure: Leveraging Electronic Health Record Screening Tools THE CASE FOR ROUTINE SCREENING Iron deficiency (ID) is one of the most common comorbidities in heart
Screening and Diagnosis of ID in HF
Screening and Diagnosis of ID in HF Challenges With the Diagnosis of Iron Deficiency in Heart Failure Iron deficiency (ID) is a very common comorbidity in patients with heart failure

Treatment and Recent Trials of ID in HF
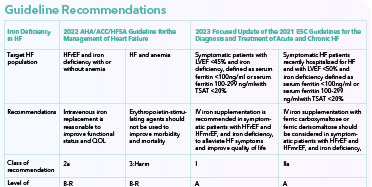
The Treatment of Iron Deficiency in Heart Failure: Options, Guideline Recommendations, and Recent Developments THE SCOPE OF THE PROBLEM For patients with heart failure (HF), iron deficiency (ID) is an
Expert Perspectives

Gurusher Panjrath, MD, FACC, FAHA

Ileana L Piña, MD, MPH, FAHA, FACC, FHFSA

Katherine E. Di Palo, PharmD, MBA, MS, FAHA, FHSA

Javed Butler, MD, MPH, MBA
- Burden and Causes of ID in HF
- Clinical Manifestations, Screening and Diagnosis of ID in HF
- Inadequacy of Oral Iron to Treat ID in HF
- IV Iron Therapy to Treat ID in HF: a Review of Key Trials
- IV Iron therapy for ID in HF: Guideline Updates, Meta-analysis, and Ongoing Trials
- Panel Discussion: Addressing ID in HF
- Concerns from Patients
- Importance of treatment of ID in HF
- Take-home Messages
- ID in HF: The Role of Clinical Decision Support Tools
Provider Resources
Causes of ID
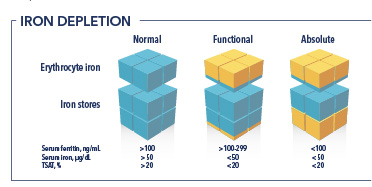
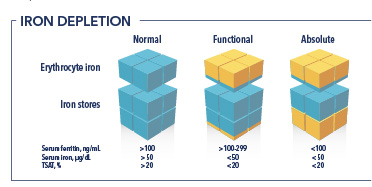
Iron has both a storage pool and a functional pool. ID can be absolute (the body’s iron store is empty) or functional (when the release of iron is compromised).
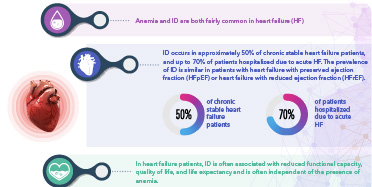
Prevalence of ID in HF
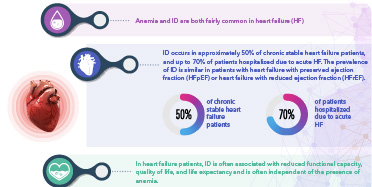
ID occurs in approximately 50% of chronic stable heart failure patients, and up to 70% of patients hospitalized due to acute HF.
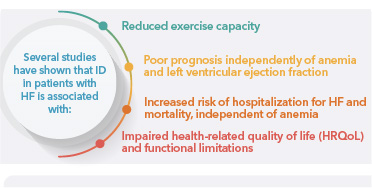
Impact of ID in Heart Failure
ID in patients with stable systolic heart failure has been observed to be associated with submaximal exercise capacity as well as endurance.
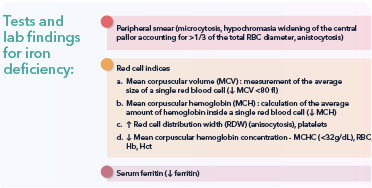
Tests and Diagnosis Of ID
Algorithm for Screening, Diagnosis and Treatment Decision for ID in Patients with Heart Failure
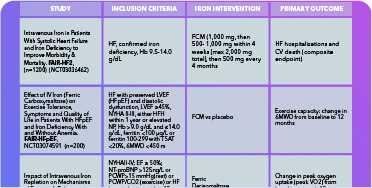
Ongoing Clinical Trials for ID in HF
Outline of ongoing trials & major publications assessing effects of treatment of ID in chronic heart failure.
TREATMENT OF ID IN PATIENTS
Algorithm for screening/diagnosis and treatment/follow‐up of ID in patients with chronic HF.
Causes of ID
Iron has both a storage pool and a functional pool. ID can be absolute (the body’s iron store is empty) or functional (when the release of iron is compromised).
Prevalence of ID in HF
ID occurs in approximately 50% of chronic stable heart failure patients, and up to 70% of patients hospitalized due to acute HF.
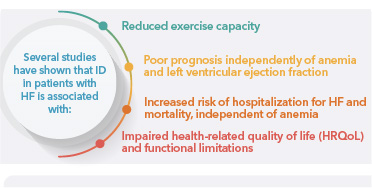
Impact of ID in Heart Failure
ID in patients with stable systolic heart failure has been observed to be associated with submaximal exercise capacity as well as endurance.
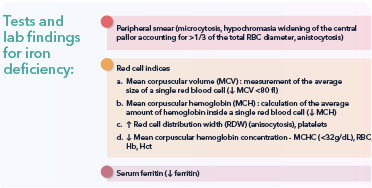
Tests and Diagnosis Of ID
Algorithm for Screening, Diagnosis and Treatment Decision for ID in Patients with Heart Failure
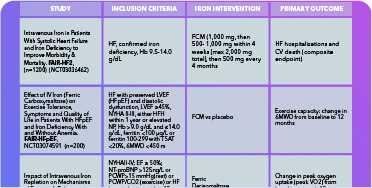
Ongoing Clinical Trials for ID in HF
Outline of ongoing trials & major publications assessing effects of treatment of ID in chronic heart failure.
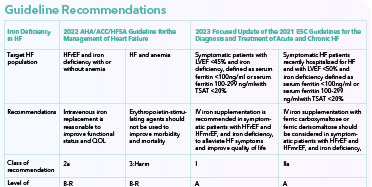
Treatment of ID in Patients
Algorithm for screening/diagnosis and treatment/follow‐up of ID in patients with chronic HF.

The Role of Clinical Decision Support Tools
A slide resource reviewing relevant clinical decision support tools in the treatment of ID in HF.

Addressing and Treating Iron Deficiency in Patients with HF
A slide resource from a recent 2023 webcast recording reviewing how to address and treat iron deficiency in HF patients.
Clinician Resources & Suggested Readings
2
4
5
8
Patient Resources
How is Iron Deficiency diagnosed and treated?
Iron deficiency is determined by the value of lab markers in your blood. Talk to your doctor if your lab values are below normal
Know Iron Deficiency in Heart Failure
Iron makes hemoglobin, a part of red blood cells that carries oxygen to tissues
Iron is an important mineral our bodies need to make hemoglobin (Hgb), a protein in red blood cells that carries oxygen from our lungs to other parts of our bodies. Iron is also used to make the protein myoglobin, which helps with storing and providing oxygen to muscles. Iron also helps make and break down specific proteins and hormones, as well as repair our DNA. Additionally, iron plays a role in a healthy immune system.
References:
- Alnuwaysir RIS, Hoes MF, van Veldhuisen DJ, van der Meer P, Grote Beverborg N. Iron deficiency in heart failure: mechanisms and pathophysiology. J Clin Med. 2021;11(1):125. Published 2021 Dec 27. doi:10.3390/jcm11010125
ID occurs when the body’s iron stores are too low, which may have a negative effect on different body processes, including making Hgb and healthy red blood cells. Without enough iron, our red blood cells may not provide enough oxygen to tissues and organs. ID can worsen and become iron deficiency anemia (IDA), in which our bodies cannot make enough healthy red blood cells. You may have lower iron levels if you have HF. ID is very common in HF patients, with 60-80% of HF patients having ID. Having HF may increase your risk of ID, and having ID may be linked to worse effects from your HF condition, including worse symptoms, lower quality of life, and higher risk of hospital visits and death.
References:
- Harvard T.H. Chan School of Public Health. The Nutrition Source. Accessed September 21, 2023. https://www.hsph.harvard.edu/nutritionsource/iron/
- Alnuwaysir RIS, Hoes MF, van Veldhuisen DJ, van der Meer P, Grote Beverborg N. Iron deficiency in heart failure: mechanisms and pathophysiology. J Clin Med. 2021;11(1):125. Published 2021 Dec 27. doi:10.3390/jcm11010125
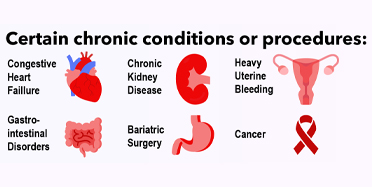
ID most likely occurs in HF patients due to one or more of these reasons: (1) not enough intake of iron in our diets; (2) inability of our bodies to absorb enough iron; and/or (3) iron loss through abnormal bleeding. Individuals with HF may find it more difficult to consume recommended amounts of iron due to fatigue, shortness of breath, or reduced appetite. HF can also cause body inflammation and changes in our intestines, making it harder to absorb iron. Compared to the general population, HF patients may also be more vulnerable to iron loss through bleeding in the stomach or intestines.
References:
- Savarese G, von Haehling S, Butler J, Cleland JGF, Ponikowski P, Anker SD. Iron deficiency and cardiovascular disease. Eur Heart J. 2023;44(1):14-27. doi:10.1093/eurheartj/ehac569
- Alnuwaysir RIS, Hoes MF, van Veldhuisen DJ, van der Meer P, Grote Beverborg N. Iron deficiency in heart failure: mechanisms and pathophysiology. J Clin Med. 2021;11(1):125. Published 2021 Dec 27. doi:10.3390/jcm11010125
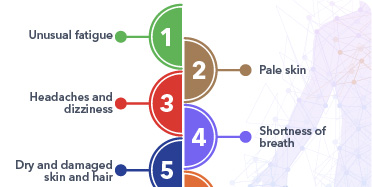
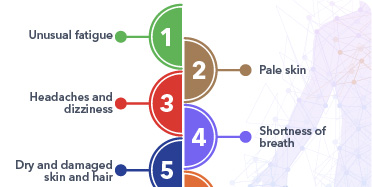
Symptoms of ID may include fatigue, weakness, body aches, shortness of breath, pale skin, sensitivity to cold, brittle fingernails, hair loss, headaches, dizziness, trouble sleeping or concentrating. Extreme or constant fatigue, severe dizziness or fainting, confusion, rapid heartbeat, or chest pain can be symptoms of severe ID; it is important to speak with your health care provider immediately if you experience any of these symptoms.
References:
- Mayo Clinic. Iron deficiency anemia.Accessed September 22, 2023. https://www.mayoclinic.org/diseases-conditions/iron-deciency-anemia/symptoms-causes/syc-20355034
- Harvard T.H. Chan School of Public Health. The Nutrition Source. Accessed September 22, 2023. https://www.hsph.harvard.edu/nutritionsource/iron.
If your health care provider suspects you may have ID, they can perform blood tests to help make a diagnosis. These tests include ferritin and transferrin saturation (TSAT). Ferritin is a protein in the blood that stores iron until it is needed by the body. A ferritin test will determine how much iron your body has in storage. Transferrin is a protein that transports iron. A TSAT test will show how much transferrin is available to move iron within your body. If your provider suspects that you may have IDA, additional tests including Hgb will also be ordered to evaluate the health of your red blood cells.
References:
- Mayo Clinic. Iron deficiency anemia.Accessed September 22, 2023. https://www.mayoclinic.org/diseases-conditions/iron-deciency-anemia/symptoms-causes/syc-20355034
- Alnuwaysir RIS, Hoes MF, van Veldhuisen DJ, van der Meer P, Grote Beverborg N. Iron deficiency in heart failure: mechanisms and pathophysiology. J Clin Med. 2021;11(1):125. Published 2021 Dec 27. doi:10.3390/jcm11010125
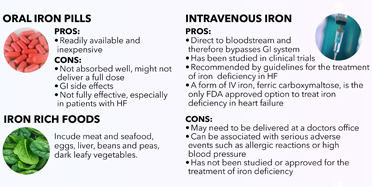
Your health care provider can discuss different options for ID treatment with you. The most highly recommended method to increase iron levels quickly and effectively is by delivering iron directly into your blood stream through intravenous (IV) infusion. IV iron has shown to improve functional status, quality of life, and decrease the risk of HF hospitalizations in clinical trials. A form of IV iron, ferric carboxymaltose, is the only FDA approved option to treat iron deficiency in heart failure.
While it is possible to take an iron tablet, iron taken by mouth is not well absorbed, especially in patients with HF, and often causes stomach and intestinal problems like constipation. As this method does not improve iron levels to the same degree as IV iron, it is generally not the treatment of choice.
References:
- Beavers CJ, Ambrosy AP, Butler J, et al. Iron Deficiency in Heart Failure: A scientific statement from the Heart Failure Society of America. J Card Fail. 2023;29(7):1059-1077. doi:10.1016/j.cardfail.2023.03.025
- Anand IS, Gupta P. Anemia and Iron Deficiency in Heart Failure: Current concepts and emerging therapies. Circulation. 2018;138(1):80-98. doi:10.1161/CIRCULATIONAHA.118.030099
There are many foods you can eat to help boost your iron levels. The sources of iron best absorbed by the body include: meats, especially liver and organ meat, and seafood such as canned sardines and tuna. Other sources include: beans, lentils, nuts, seeds, spinach, potato with skin, and dark chocolate. Consuming iron-rich foods with vitamin C-containing foods like lemons, oranges or tomatoes can increase iron absorption. It can take a long time to increase iron levels through diet alone, so if your iron levels are too low, treatment such as with IV iron may be recommended. Certain drinks such as tea, coffee, red wine and milk may interfere with iron absorption, so it is best to avoid these drinks with meals.
References
- Harvard T.H. Chan School of Public Health. The Nutrition Source. Accessed September 22, 2023. https://www.hsph.harvard.edu/nutritionsource/iron/
- Milman NT. A review of nutrients and compounds, which promote or inhibit intestinal iron absorption: making a platform for dietary measures that can reduce iron uptake in patients with genetic haemochromatosis. J Nutr Metab. 2020;2020:7373498. Published 2020 Sep 14. doi:10.1155/2020/7373498